Correlation between Carotid Artery Fat Density and Atherosclerosis
-
摘要:
目的:本文旨在探讨颈动脉周围脂肪密度与动脉粥样硬化型狭窄及脑缺血事件的相关性,为颈动脉粥样硬化型狭窄的早期识别提供临床参考。方法:回顾性收集盘锦市中心医院2023年1月至2023年8月接受颈动脉计算机断层血管成像(CTA)检查具有完整临床资料有明确诊断的患者,共224侧血管纳入研究,根据是否有动脉粥样硬化分为狭窄组及对照组,狭窄组细分为轻度、中重度狭窄,根据不同年龄划分为Ⅰ、Ⅱ、Ⅲ组,根据患者有无症状分为有症状组及无症状组,探讨血管周围脂肪密度(PFD)与颈动脉粥样硬化型狭窄及脑血管事件的相关性。结果:临床资料中高血压、高血脂及年龄与颈动脉粥样硬化狭窄有关,差异有统计学意义。随颈动脉狭窄程度的加重,颈动脉PFD会逐渐升高。PFD随年龄增长而逐渐增加。相关性分析显示:PFD、年龄、高血压病史、高血脂病史与颈动脉狭窄间存在正相关。狭窄侧血管有症状组PFD高于无症状组,二元Logistic矫正混杂因素后差异仍有统计学意义。结论:颈动脉PFD是颈动脉粥样硬化型狭窄的独立危险因素,且症状性颈动脉狭窄患者颈动脉周围脂肪密度高。
Abstract:Objective: In this study, we aim to investigate the correlation between carotid artery fat density and atherosclerotic stenosis, providing a clinical reference for the early identification of carotid atherosclerotic stenosis. Methods: A retrospective analysis was conducted on patients with complete clinical data and confirmed diagnoses who underwent carotid computed tomography angiography (CTA) at Panjin Central Hospital between January 2023 and August 2023. A total of 224 blood vessels were included in the study. Patients were divided into a stenosis group and a control group based on the presence or absence of atherosclerosis. The stenosis group was further categorized into mild, moderate, and severe stenosis, and classified into Groups I, II, and III based on age. Additionally, patients were classified into symptomatic and asymptomatic groups based on their symptom status, and the correlation between perivascular fat density (PFD), carotid atherosclerotic stenosis, and cerebrovascular events was explored. Results: Hypertension, hyperlipidemia, and age were significantly associated with carotid atherosclerotic stenosis. PFD increased with the degree of stenosis and age. Correlation analysis revealed a positive correlation between PFD, age, history of hypertension, history of hyperlipidemia, and carotid artery stenosis. The PFD in the symptomatic group was higher than in the asymptomatic group, and the difference remained statistically significant after binary logistic correction for confounding factors. Conclusion: Carotid artery PFD is an independent risk factor for carotid atherosclerotic stenosis. Patients with symptomatic carotid artery stenosis exhibit higher carotid fat density compared to their asymptomatic counterparts.
-
-
表 1 患者一般情况比较
Table 1 Comparison of general conditions of patients
指标 狭窄组(n=111) 对照组(n=113) Z/$\chi^2 $ P 性别,男性 73.87%(82/29) 63.72%(72/41) 2.689 0.101 年龄/岁 65(57,72) 57(46,65.5) 5.026 < 0.001 高血压 70.27%(78/33) 50.44%(57/56) 9.193 0.002 糖尿病 16.22%(18/93) 20.35%(23/90) 0.641 0.423 高同型半胱氨酸 7.21%(8/103) 2.65%(3/110) 2.485 0.115 高血脂 14.41%(16/95) 5.31%(6/107) 5.241 0.022 烟酒史 12.61%(14/97) 6.19%(7/106) 2.715 0.099 冠心病 13.51%(15/96) 7.96%(9/104) 1.802 0.179 PFD/HU −71.61(−77.55,−66.84) −82.96(−86.23,−79.61) 10.334 < 0.001 表 2 不同狭窄程度PFD比较
Table 2 Comparison of PFD across different degrees of stenosis
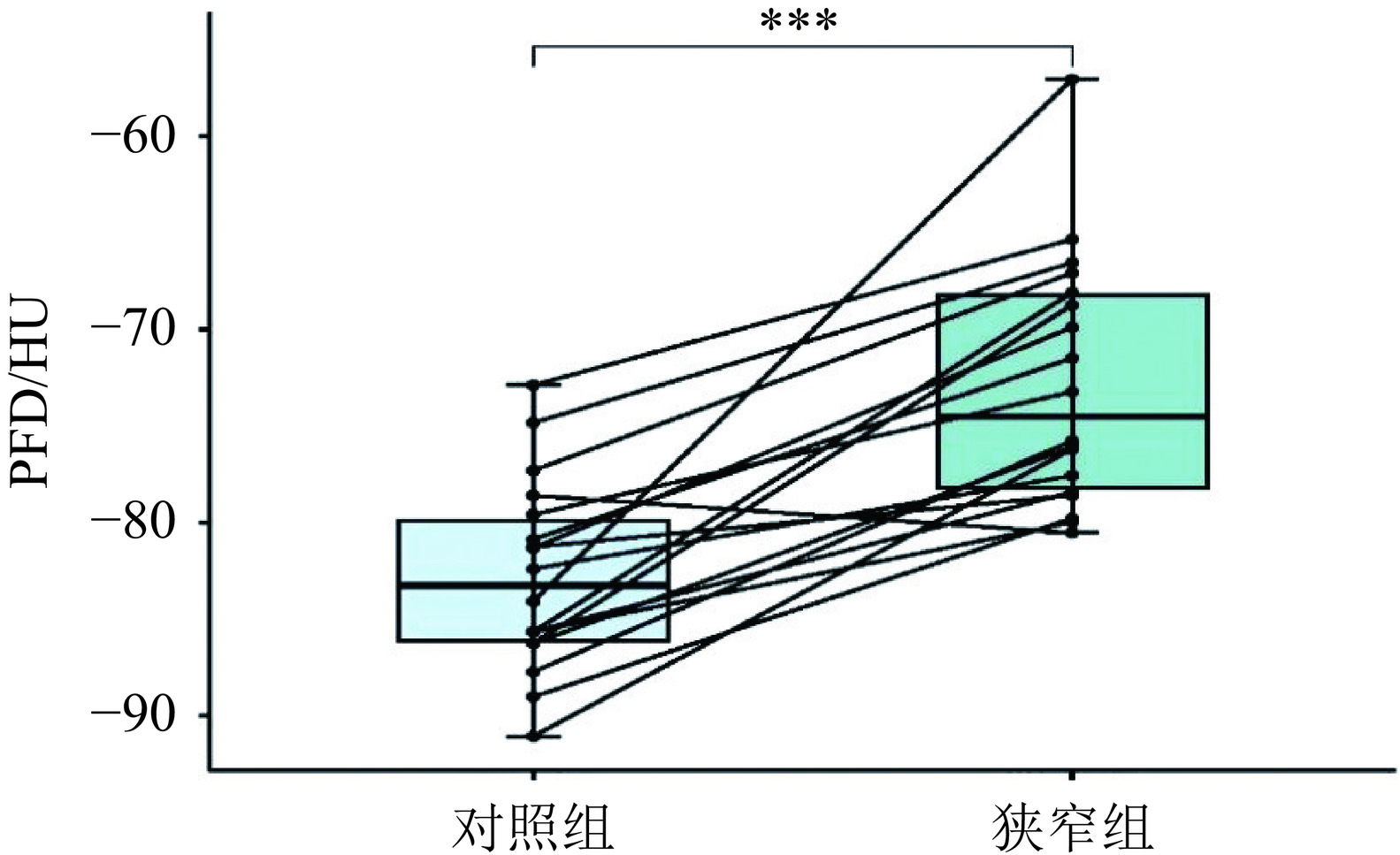
组别 对照组(n=113) 轻度狭窄组(n=81) 中重度狭窄(n=30) H P PFD −82.96(−86.32,−79.61) −75.08(−77.96,−69.38) ▲ −65.64(−69.37,−59.61)*# 114.911 < 0.001 注:*表示对照组与中重度狭窄组相比P < 0.05;#表示轻度狭窄组与中重度狭窄组相比P < 0.05;▲表示对照组与轻度狭窄组相比P < 0.05。 表 3 同一患者狭窄组与对照组PFD比较
Table 3 Comparison of PFD between stenosis and control groups in the same patients
组别 狭窄组(n=18) 对照组(n=18) t P值 PFD均值 −72.79±6.43 −82.79±4.90 6.59 < 0.001 表 4 不同年龄段PFD比较
Table 4 Comparison of PFD across different age groups
Ⅰ组(n=30) Ⅱ组(n=103) Ⅲ组(n=91) H P值 PFD −82.46(−86.14,−78.55) −78.75(−83.69,−72.69)▲ −76.53(−80.01,−67.82)*# 17.743 < 0.001 注:Ⅰ组与Ⅲ组相比*P < 0.05;Ⅱ组与Ⅲ组相比#P < 0.05;Ⅰ组与Ⅱ组相比▲P < 0.05。 表 5 各指标与颈动脉狭窄的相关性分析
Table 5 Correlation analysis between various indices and carotid artery stenosis
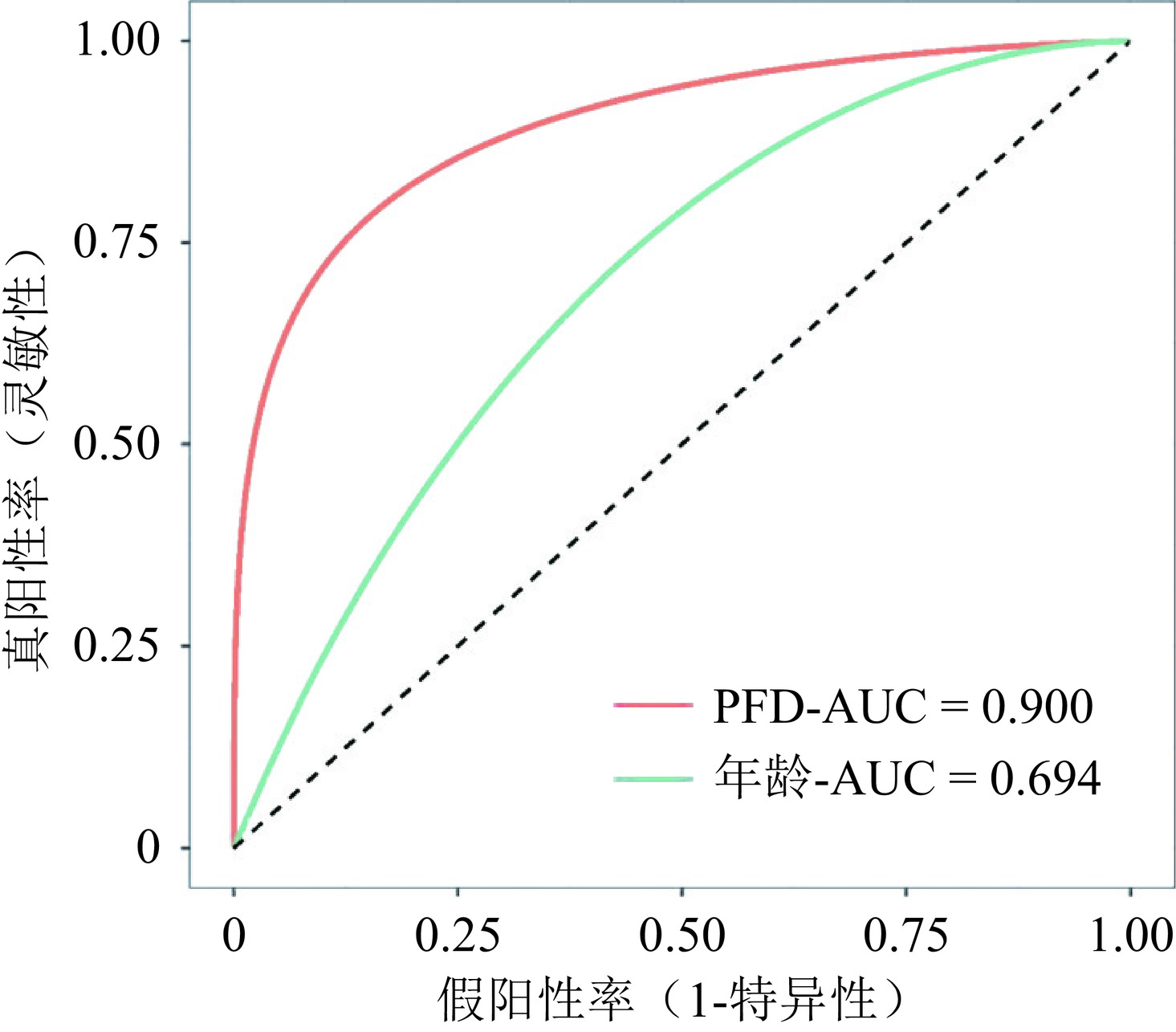
指标 r P PFD 0.692 < 0.001 年龄 0.337 < 0.001 性别 0.110 0.101 冠心病 0.090 0.179 高血脂 0.153 0.022 高同型半胱氨酸 0.105 0.115 糖尿病 −0.053 0.426 烟酒史 0.110 0.099 高血压 0.203 0.002 表 6 二元Logistic回归分析
Table 6 Binary logistic regression analysis
调整前 调整后 OR 95%CI P OR 95%CI P PFD 1.366 1.258-1.485 < 0.001 1.357 1.242-1.484 < 0.001 年龄 1.070 1.042-1.099 < 0.001 1.045 1.009-1.083 0.014 表 7 有症状与无症状患者PFD均值比较
Table 7 Comparison of mean PFD between symptomatic and asymptomatic patients
PFD 有症状 无症状 Z P 狭窄组 −68.74(−76.96,−64.52) −74.97(−77.71,−69.43) −2.327 0.020 对照组 −83.00(−86.25,−79.91) −82.74(−86.05,−79.00) −0.367 0.714 表 8 狭窄组中有症状与无症状患者二元Logistic回归
Table 8 Binary logistic regression analysis of symptomatic and asymptomatic patients in the stenosis group
调整前 调整后 OR 95%CI P OR 95%CI P PFD 1.060 1.010-1.113 0.019 1.073 1.013-1.136 0.017 -
[1] LIU H H, JING J, WANG A X, ET AL. Stroke recurrence and antiplatelets in posterior versus anterior circulation minor stroke or transient ischemic attack[J]. Stroke, 2023, 54(4): 964-972. DOI: 10.1161/STROKEAHA.122.041738.
[2] WAKSMAN R, MERDLER I, PATEL P, ET AL. Targeting inflammation in atherosclerosis: overview, strategy and directions[J]. EuroIntervention, 2024, 20(1): 32-44. DOI: 10.4244/EIJ-D-23-00606.
[3] YUSUKE A, KAZUTAKA U, SEITARO N, ET AL. Beiging of perivascular adipose tissue regulates its inflammation and vascular remodeling[J]. Nature Communications, 2022, 13(1): 5117. DOI: 10.1038/s41467-022-32658-6.
[4] QI X Y, QU S L, XIONG W H, ET AL. Perivascular adipose tissue (PVAT) in atherosclerosis: a double-edged sword[J]. Cardiovascular diabetology, 2018, 17(1): 1-20. DOI: 10.1186/s12933-017-0656-x.
[5] CHENG C K, DING H, JIANG M, ET AL. Perivascular adipose tissue: Fine-tuner of vascular redox status and inflammation[J]. Redox Biology, 2023, 20(4): 102683.
[6] 冉值祯, 马跃, 侯阳. 心外膜脂肪组织密度对冠状动脉粥样硬化性心脏病的诊断价值[J]. 中国现代医学杂志, 2022, 32(1): 47-51. DOI: 10.3969/j.issn.1005-8982.2022.01.009. RAN Z Z, MA Y, HOU Y. Diagnostic value of epicardial adipose tissue density in coronary atherosclerotic heart disease[J]. China Journal of Modern Medicine, 2022, 32(1): 47-51. DOI: 10.3969/j.issn.1005-8982.2022.01.009. (in Chinese).
[7] MA R, VAN ASSEN M, SIDORENKOV G, ET AL. Relationships of pericoronary and epicardial fat measurements in male and female patients with and without coronary artery disease[J]. European Journal of Radiology, 2023, 169: 111154. DOI: 10.1016/j.ejrad.2023.111154.
[8] MANUBOLU V S, LU J Y, MONTANO B, et al. Exploring the relationship between epicardial fat and coronary plaque burden and characteristics: Insights from cardiac CT imaging[J]. The International Journal of Cardiovascular Imaging. 2024, 40(9): 1951-1959.
[9] 孙万京, 仲玲珊, 李春阳, 等. 颈动脉分叉角同颈内动脉起始处粥样硬化的相关性[J]. 影像研究与医学应用, 2019, 3(7): 221. DOI: 10.3969/j.issn.2096-3807.2019.07.155. SUN W J, ZHONG L S, LI C Y, ET AL. Correlation between carotid bifurcation Angle and atherosclerosis at the beginning of internal carotid artery[J]. Imaging Research and Medical Applicati on, 2019, 3(7): 221. DOI: 10.3969/j.issn.2096-3807.2019.07.155. (in Chinese).
[10] 余苗, 孟闫凯, 徐含波, 等. 颈动脉周围脂肪密度与急性缺血性脑卒中事件的相关性研究[J]. 临床放射学杂志, 2023, 42(6): 910-914. YU M, MENG Y K, XU H B, ET AL. Correlation between peripheral carotid fat density and acute ischemic stroke[J]. Journal of Clinical Radiology, 2023, 42(6): 910-914. (in Chinese).
[11] HEDIYEH B, K P M, PRANEIL P, ET AL. Association between carotid artery perivascular fat density and cerebrovascular ischemic events[J]. Journal of the American Heart Association, 2018, 7(24): 10383-10387.
[12] 中国心血管健康与疾病报告2022概要[J]. 中国循环杂志, 2023, 38(6): 583-612. The Writing Committee of the Report on Cardiovascular Health and Diseases in China[J]. Chinese Circulation Journal, 2023, 38(6): 583-612. (in Chinese).
[13] FLAHERTY M L, KISSELA B, KHOURY J C, ET AL. Carotid artery stenosis as a cause of stroke[J]. Neuroepidemiology, 2013, 40(1): 36-41. DOI: 10.1159/000341410.
[14] CHENG S F, BROWN M M, SIMISTER R J, ET AL. Contemporary prevalence of carotid stenosis in patients presenting with ischaemic stroke[J]. The British Journal of Surgery, 2019, 106(7): 872-878. DOI: 10.1002/bjs.11136.
[15] SONG P G, FANG Z, WANG H Y, ET AL. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: A systematic review, meta-analysis, and modelling study[J]. Lancet Glob Health, 2020, 8(5): 721-729. DOI: 10.1016/S2214-109X(20)30117-0.
[16] AKIHIRO N, TOMOYO S, MAKOTO A, ET AL. Plaque Rupture, compared with plaque erosion, is associated with a higher level of pancoronary inflammation[J]. JACC. Cardiovascular imaging, 2021, 15(5): 828-839.
[17] HARUHITO Y, TOMOYO S, KEISHI S, ET AL. Coronary inflammation and plaque vulnerability: A coronary computed tomography and optical coherence tomography study[J]. Circulation: Cardiovascular Imaging, 2023, 10(1): 59-63.
[18] CASSIE H, I A G. The pathobiology of perivascular adipose tissue (PVAT), the fourth layer of the blood vessel wall[J]. Cardiovascular pathology: the official journal of the Society for Cardiovascular Pathology, 2022, 61(1): 459-461.
[19] CAI M, ZHAO D, HAN X, ET AL. The role of perivascular adipose tissue-secreted adipocytokines in cardiovascular disease[J]. Frontiers in immunology, 2023, 14(1): 49-51.
[20] RYSZARD N, J T G. Perivascular adipose tissue inflammation in vascular disease[J]. British journal of pharmacology, 2017, 174(20): 3496-3513. DOI: 10.1111/bph.13705.
[21] BERMAN DS, KWIECINSKI J. Imaging coronary inflammatory risk[J]. JACC. Cardiovascular imaging, 2021, 15(3): 472-475.
[22] OIKONOMOU E K, ANTONOPOULOS A S, SCHOTTLANDER D, ET AL. Standardized measurement of coronary inflammation using cardiovascular computed tomography: integration in clinical careas a prognostic medical device[J]. Cardiovascular research, 2021, 117(13): 2677-2690.
[23] HU X, CHEN J, FU H, ET AL. Association between carotid artery perivascular fat density and embolic stroke of undetermined source[J]. Frontiers in Neurology, 2022, 12(1): 765962.
[24] 牛稳, 邱晓晖, 刘艺超. 颈动脉粥样硬化狭窄的血管周围脂肪密度与脑梗死之间的关系[J]. 实用医学杂志, 2023, 39(1): 103-108. NIU W, QIU X H, LIU Y C. The relationship between perivascular fat density and cerebral infarction in carotid atherosclerosis[J]. Journal of Practical Medicine, 2023, 39(1): 103-108. (in Chinese).
[25] SABA L, ZUCCA S, GUPTA A, ET AL. Perivascular fat density and contrast plaque enhancement: does a correlation exist[J]. AJNR Am J Neuroradiol, 2020, 41(8): 1460-1465 DOI: 10.3174/ajnr.A6710.
[26] ZHANG D H, JIN J L, ZHU C F, ET AL. Association between carotid artery perivascular fat density and cerebral small vessel disease[J]. Aging, 2021, 13(14): 839-851.
[27] HENRICHOT E, JUGE-AUBRY C E, PERNIN A, ET AL. Production of chemokines by perivascular adipose tissue: A role in the pathogenesis of atherosclerosis[J]. Arteriosclerosis, Thrombosis, and Vascular Biology, 2005, 25(12): 2594-2599. DOI: 10.1161/01.ATV.0000188508.40052.35.
[28] USUI E, MATSUMURA M, MINTZ G S, ET AL. Clinical outcomes of low-intensity area without attenuation and cholesterol crystals in non-culprit lesions assessed by optical coherence tomography[J]. Atherosclerosis, 2021, 332(1): 41-47.
[29] OIKONOMOU E K, MARWAN M, DESAI M Y, ET AL. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data[J]. Lancet, 2018, 392(10151): 929-939. DOI: 10.1016/S0140-6736(18)31114-0.
[30] 应伟峰, 陈穹, 张莹, 等. 冠状动脉易损与非易损斑块的冠周与主动脉根部心外膜脂肪CT衰减指数比值差异[J]. 中国医学影像学杂志, 2023, 31(8): 818-823. DOI: 10.3969/j.issn.1005-5185.2023.08.005. YING W F, CHEN Q, ZHANG Y, ET AL. The difference of CT attenuation index ratio between pericardial and epicardial fat in vulnerable and non-vulnerable coronary plaques[J]. Chinese Journal of Medical Imaging, 2023, 31(8): 818-823. DOI: 10.3969/j.issn.1005-5185.2023.08.005.
[31] MUSHENKOVA N V, SUMMERHILL V I, ZHANG D, ET AL. Current advances in the diagnostic imaging of atherosclerosis: insights into the pathophysiology of vulnerable plaque[J]. International Journal of Molecular Sciences, 2020, 21(8): 2992. DOI: 10.3390/ijms21082992.
[32] 李静, 乔建民, 王俊奇, 等. 心外膜及心周脂肪体积与颈动脉粥样斑块的关系[J]. CT理论与应用研究, 2017, 26(6): 761-768. LI J, QIAO J M, WANG J Q, ET AL. Relationship between epicardial and pericardiac fat volume and carotid atherosclerotic plaque[J]. CT Theoretical and Applied Research, 2017, 26(6): 761-768.
[33] ANTONOPOULOS AS, SANNA F, SABHARWAL N, ET AL. Detecting human coronary inflammation by imaging perivascular fat[J]. Science Translational Medicine, 2017, 9(398): 2658. DOI: 10.1126/scitranslmed.aal2658.
[34] BARADARAN H, MYNENI P K, PATEL P, ET AL. Association between carotid artery perivascular fat density and cerebrovascular ischemic events[J]. Journal of the American Heart Association, 2018, 7(24): e010383. DOI: 10.1161/JAHA.118.010383.
[35] XIA R, FAN S, JIAN H, ET AL. Impact of carotid hemodynamics on carotid plaque location: Age difference[J]. Neuro endocrinology letters, 2023, 44(6): 399-409.




 下载:
下载: