Diagnostic Value of CT-detected Extramural Vessel Invasion in Lymph Node Metastasis of Gastric Cancer
-
摘要:
目的:探讨胃癌壁外血管侵犯MDCT表现对淋巴结转移的诊断价值。方法:回顾性收集2020年1月至2022年6月经手术病理证实的105例胃癌患者;所有患者CT扫描后2周内行根治性胃癌切除术与D2淋巴结清扫术;门脉期MDCT图像上采用5分量表对胃癌EMVI情况进行评估;根据病理淋巴结转移情况将患者分为淋巴结转移组与非淋巴结转移组。比较两组间临床病理特征差异,多因素Logistic回归分析胃癌淋巴结转移的影响因素,受试者操作特征(ROC)曲线用于评估ctEMVI对淋巴结转移的诊断价值,比较ctEMVI和淋巴结短径对淋巴结转移的诊断价值。结果:淋巴结转移组中,脉管侵犯占60.9%(39例),肿瘤大小(>5 cm)占64.1%(41例),ctEMVI阳性占79.7%(51例),CT转移性淋巴结阳性占56.2%(36例);非淋巴结转移组中,脉管侵犯,肿瘤大小(>5 cm),ctEMVI阳性及CT转移性淋巴结阳性分别占21.9%(9例),24.4%(10例),21.9%(9例)和19.5%(8例),两组间的差异均有统计学意义;多因素logistic回归分析显示ctEMVI是淋巴结转移的独立影响因素;ROC曲线显示ctEMVI诊断淋巴结转移的AUC为0.854。ctEMVI诊断淋巴结转移的敏感性,准确性优于淋巴结短径。结论:ctEMVI是淋巴结转移的独立影响因素,ctEMVI在诊断淋巴结转移方面具有重要价值。
Abstract:Objective: To investigate the diagnostic value of extramural vessel invasion (EMVI) in multidetector row computed tomography (MDCT) of lymph node metastasis of gastric cancer. Methods: A total of 105 patients with pathologically confirmed gastric cancer treated at our hospital between January 2020 and June 2022 were retrospectively collected. All patients underwent radical gastrectomy and D2 lymph node dissection within 2 weeks after the CT scan. The EMVI status of gastric cancer was evaluated on portal-phase MDCT images using a 5-point scale. According to the pathological status of lymph node metastasis, the patients were divided into lymph node and non-lymph node metastasis groups, and their clinicopathologic features were compared. We then performed a multivariate logistic regression analysis of lymph node metastasis in gastric cancer. A receiver operating characteristic (ROC) curve was used to evaluate the diagnostic value of CT-detected EMVI (ctEMVI) in lymph node metastasis, and the diagnostic values of ctEMVI and lymph node short diameter in lymph node metastasis were compared. Results: In the lymph node metastasis group, lymphovascular invasion, tumor size (>5 cm), ctEMVI positivity, and CT metastatic lymph node positivity accounted for 60.9% (n=39), 64.1% (n=41), 79.7% (n=51), and 56.2% (n=36) of cases, respectively. In the non-metastatic group, lymphovascular invasion, tumor size (>5 cm), ctEMVI positivity, and CT metastatic lymph node positivity accounted for 21.9% (n=9), 24.4% (n=10), 21.9% (n=9), and 19.5% (n=8), respectively. The intergroup difference was statistically significant. The multivariate logistic regression analysis showed that ctEMVI was an independent factor of lymph node metastasis. The ROC curve showed that the area under the curve of ctEMVI for diagnosing lymph node metastasis was 0.854. The sensitivity and accuracy of ctEMVI were superior to those of lymph node short diameter in the diagnosis of lymph node metastasis. Conclusion: This study found that ctEMVI was an independent factor and of great value in the diagnosis of lymph node metastasis.
-
Keywords:
- CT /
- extramural vessel invasion /
- gastric cancer /
- lymph node metastasis
-
胃癌是消化系统常见恶性肿瘤,其早期临床症状隐匿,患者就诊时多为进展期胃癌,临床预后通常不佳[1]。淋巴结转移是胃癌常见转移途径,与患者治疗方案制定及临床预后有关[2]。
壁外血管侵犯(extramural vessel invasion,EMVI)是胃癌常见的转移方式,它是指肿瘤细胞侵入固有肌层外的静脉血管[3]。MRI已在直肠癌EMVI诊断中得到广泛应用。有研究表明mrEMVI是肿瘤患者临床预后不佳的独立预测因子,与肿瘤高复发率及转移率有关[4]。然而MRI价格昂贵,扫描时间长,易受胃蠕动的影响,目前难以作为胃癌患者的术前常规影像学检查。多层螺旋CT(multidetector CT,MDCT)作为胃癌患者术前常规影像学检查,拥有高分辨率图像及多平面重建技术,可对EMVI进行准确术前识别[5]。目前有关胃癌EMVI的术前影像学研究报道不多,本研究旨在探讨胃癌壁外血管侵犯MDCT表现对淋巴结转移的诊断价值。
1. 资料与方法
1.1 研究对象
回顾性收集我院2020年1月至2022年6月经手术病理证实的105例胃癌患者。
入选标准:①CT扫描后2周内行根治性胃癌切除术与D2淋巴结清扫术;②既往无胃切除术或内镜切除史;③无新辅助化疗史;④CT图像上有明确显示的病变;⑤所有患者均具备完整的术前临床影像资料与术后病理资料。排除标准:①胃切除术前接受过其他治疗;②胃切除术距离CT扫描时间超过2周;③胃充盈不佳。
1.2 仪器与方法
采用Siemens SOMATOM Sensation 64排CT,管电压120 kV,管电流自动调制,层厚及层间距均为5 mm,螺距1.0,矩阵512×512,准直1.0 mm;以流率2.5~3.0 mL/s经静脉注射对比剂碘海醇(300 mgI/mL)1.5 mL/kg体质量后行增强扫描,延迟25 s及50 s采集动脉期及静脉期图像。所有图像采集后传至Syngo.via VB20工作站,予以冠状位、矢状位、横断位重建(重建层厚1.0 mm)。
1.3 图像分析
由两位高年资影像医师在未知病理结果的情况下观察并分析图像,图像序列包括:门脉期横断位、矢状位及冠状位重建图像。若两位医师阅片结果出现不一致的情况,则由第3位高年资影像医师进行再次阅片判断。
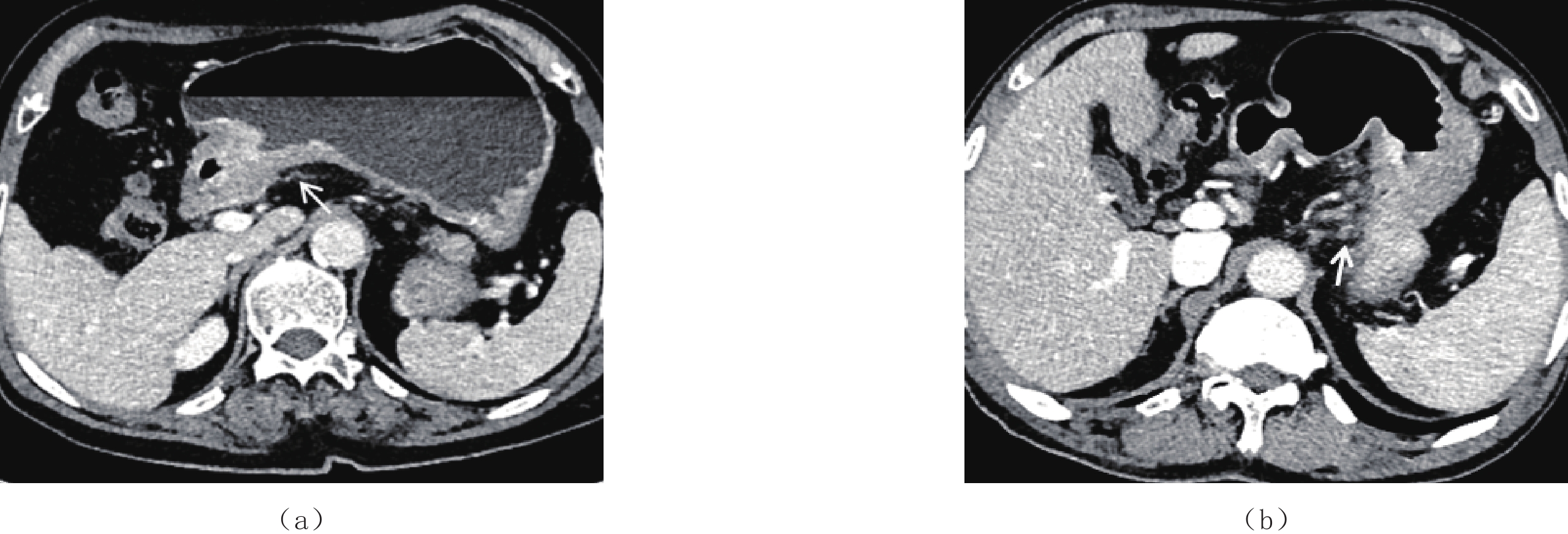
根据直肠癌高分辨MR图像所定义的EMVI评分标准[6],在门脉期图像上采用5分量表对胃癌EMVI情况进行评估。0分:肿瘤侵犯胃壁,但外轮廓光滑,病灶周围无血管;1分:肿瘤穿透胃壁呈条状向外延伸,病灶周围无血管;2分:肿瘤穿透胃壁呈条状向外延伸,病灶周围见血管,血管管腔正常且腔内无类似肿瘤密度影;3分:肿瘤穿透胃壁呈条状向外延伸,病灶周围血管管腔内可见类似肿瘤密度影,血管管径增宽;4分:肿瘤周围血管管腔内可见类似肿瘤密度影,血管轮廓不规则或管腔结节样扩张。0~2分为ctEMVI阴性,3~4分为ctEMVI阳性(图1)。
MDCT静脉期横断位图像上测量胃周各组淋巴结的短径,以淋巴结短径>8 mm作为CT转移性淋巴结的诊断标准[7]。MDCT横断位图像上测量肿瘤最长径作为肿瘤大小。
1.4 病理分析
胃癌的组织病理学特征由两位经验丰富的胃肠病理学家进行评估,意见不一致者经协商后解决。肿瘤的分化程度及脉管侵犯情况被记录。
根据AJCC第8版TNM分期系统对淋巴结清扫术后标本进行准确的N分期。根据N分期结果,将患者分为淋巴结转移组和非淋巴结转移组。
1.5 统计学分析
符合正态分布的计量资料以(均数±标准差)表示,两组间比较采用独立样本t检验;计数资料以例(%)表示,两组间比较采用
$\chi^2 $ 检验。受试者操作特征曲线(ROC)用于评估ctEMVI对淋巴结转移的诊断价值。Kappa一致性检验用于评估ctEMVI及淋巴结短径的观察者间一致性。多因素Logistic回归分析胃癌淋巴结转移的影响因素。以病理淋巴结转移为标准,分别计算淋巴结短径及ctEMVI诊断淋巴结转移的符合率、敏感性、特异性、阳性预测值及阴性预测值。采用卡方检验比较二者符合率、敏感性、特异性、阳性预测值及阴性预测值的差异。P<0.05差异有统计学意义。
2. 结果
2.1 患者一般资料
本研究共纳入105名患者,其中男性72例,女性33例,年龄37~88岁,平均(62.4±10.6)岁。根据病理淋巴结转移情况进行分组,淋巴结转移组64例,非淋巴结转移组41例。ctEMVI及淋巴结短径评估方面观察者间具有极好的一致性(Kappa值分别为0.841和0.852)。
2.2 淋巴结转移组与非淋巴结转移组临床病理特征比较
淋巴结转移组中,脉管侵犯占60.9%(39例),肿瘤大小(>5 cm)占64.1%(41例),ctEMVI阳性占79.7%(51例),CT转移性淋巴结阳性占56.2%(36例);非淋巴结转移组中,脉管侵犯,肿瘤大小(>5 cm),ctEMVI阳性及CT转移性淋巴结阳性分别占21.9%(9例),24.4%(10例),21.9%(9例)和19.5%(8例)。两组间的差异均有统计学意义。
两组患者年龄、性别、肿瘤位置、分化程度的差异无统计学意义(表1)。
表 1 淋巴结转移组与非淋巴结转移组临床病理特征比较Table 1. Clinicopathological features of lymph node versus non-lymph node metastasis groups指标 组别 统计检验 淋巴结转移组(n=64)(%) 非淋巴结转移组(n=41)(%) $t/\chi^2 $ P 年龄/岁 63.3±10.40 62.1±10.65 0.605 0.546 性别 男 44(68.7) 28(68.3) 0.002 0.961 女 20(31.3) 13(31.7) 肿瘤位置 胃底 10(15.6) 2(4.8) 4.786 0.091 胃体 21(32.8) 13(31.7) 胃窦 33(51.6) 26(63.5) 分化程度 低分化 34(53.1) 14(34.2) 3.695 0.158 中分化 26(40.6) 24(58.5) 高分化 4(6.3) 3(7.3) 脉管侵犯 39(60.9) 9(21.9) 15.306 <0.001 肿瘤大小/cm <5 23(35.9) 31(75.6) 15.746 <0.001 >5 41(64.1) 10(24.4) ctEMVI 阴性 13(20.3) 32(78.1) 34.016 <0.001 阳性 51(79.7) 9(21.9) CT转移性淋巴结 阴性 28(43.8) 33(80.5) 13.855 <0.001 阳性 36(56.2) 8(19.5) 2.3 logistic回归分析胃癌淋巴结转移的影响因素
经多因素Logistic回归分析显示,ctEMVI是淋巴结转移的独立影响因素(表2)。
表 2 logistic回归分析胃癌淋巴结转移的影响因素Table 2. Logistic regression analysis of factors affecting lymph node metastasis in gastric cancer指标 B WaldX2 OR 95%CI P 脉管侵犯 0.817 2.135 2.26 (0.75,6.76) 0.144 肿瘤大小 0.912 2.713 2.49 (0.84,7.36) 0.100 ctEMVI 1.916 12.207 6.79 (2.31,19.89) <0.001 CT转移性淋巴结 1.087 3.684 2.97 (0.97,8.99) 0.055 2.4 ctEMVI对淋巴结转移诊断价值分析
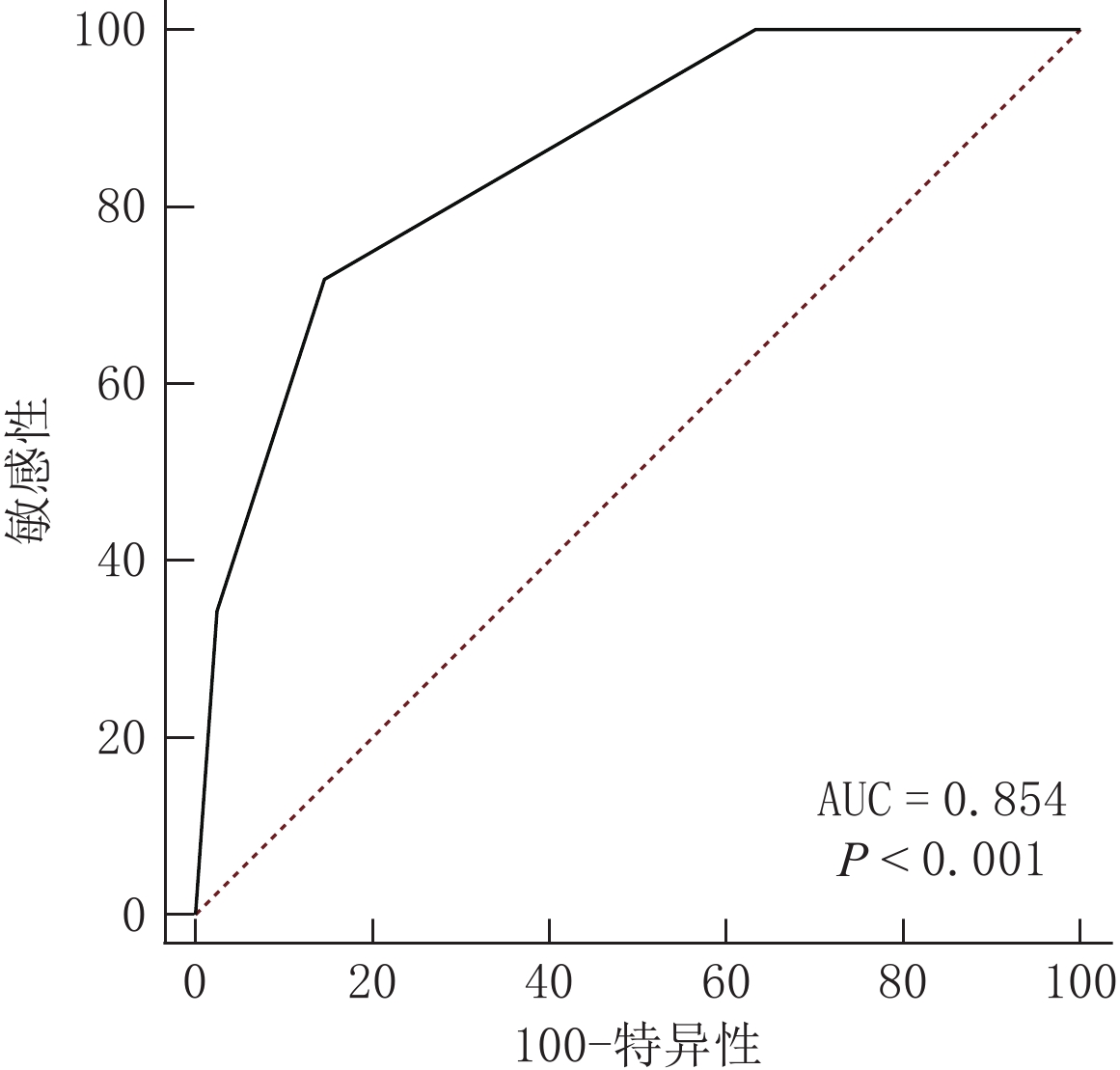
采用ROC曲线分析显示,当ctEMVI评分取截断值>2时,ctEMVI诊断转移性淋巴结的AUC值为0.854,其敏感性为79.7%,特异性为78.1%(图2)。
2.5 ctEMVI和淋巴结短径对淋巴结转移诊断价值比较
ctEMVI诊断淋巴结转移的敏感性,准确性优于淋巴结短径,差异有统计学意义(表3)。
表 3 ctEMVI与淋巴结短径对胃癌淋巴结转移的诊断价值比较Table 3. Diagnostic value of ctEMVI and lymph node short diameter on lymph node metastasis of gastric cancer指标 敏感性/% 特异性/% 阳性预测值/% 阴性预测值/% 准确性/% ctEMVI 79.7(51/64) 78.1(32/41) 85.0(51/60) 71.1(32/45) 79.1(83/105) 淋巴结短径 56.2(36/64) 80.5(33/41) 81.8(36/44) 54.1(33/61) 65.7(69/105) P 0.004 0.785 0.665 0.785 0.031 3. 讨论
淋巴结转移是影响胃癌总生存率的重要因素[2],通过术前MDCT检查评估胃癌淋巴结状态对临床治疗方案制定及判断患者预后具有重要意义。
本研究对淋巴结转移组与非淋巴结转移组的组间比较发现,肿瘤大小是淋巴结转移的影响因素,淋巴结转移组中最长径>5 cm的肿瘤所占比例较高,表明肿瘤长径是胃癌淋巴结转移的重要影响因素,与柴亚如等[8]研究结果相符。推测其原因可能是肿瘤长径越大,其与淋巴系统接触范围越大,肿瘤发生淋巴结转移的风险越高。本研究同时发现,淋巴结转移组发生脉管侵犯的风险较高,表明脉管侵犯是淋巴结转移的危险因素。肿瘤细胞一旦进入淋巴管内,其可通过淋巴回流途径发生淋巴结转移,此与胡顺航等[9]研究结果一致。
淋巴结短径是既往MDCT研究中最常见的转移淋巴结的评价指标[10]。Hasegawa等[11]研究显示,短径8 mm是判断转移性淋巴结的最佳截断值。本研究以淋巴结短径>8 mm作为转移性淋巴结的CT诊断标准,结果表明CT转移性淋巴结在淋巴结转移组与非淋巴结转移组的组间比较中具有统计学差异,这与既往文献[10]和文献[11]研究结果一致。然而本研究多变量分析显示,CT转移性淋巴结并非淋巴结转移的独立影响因素,单以淋巴结短径大小作为淋巴结转移的诊断标准并不能获得较高的准确度。有研究[12]表明,短径较小的淋巴结仍有可能发生转移,短径较大的淋巴结也可能由于炎症等原因所致。以淋巴结短径>8 mm作为诊断标准时,一定程度提高了MDCT对转移淋巴结的诊断特异性,但同时敏感性会降低[7]。因此,需要探讨新的影像评价指标以提高MDCT对淋巴结转移的诊断准确性。
既往研究[13-14]表明mrEMVI是直肠癌侧方淋巴结转移的独立影响因素。EMVI作为肿瘤沿神经血管束扩散的一种方式,其发生并不是孤立的,往往伴随着神经血管周围的淋巴侵犯。本研究显示,ctEMVI在淋巴结转移组与非淋巴结转移组的组间比较中具有统计学差异。多变量分析显示,ctEMVI是淋巴结转移的独立影响因素,与文献[13]和文献[14]报道相符。
本研究ROC曲线显示,当ctEMVI评分>2即ctEMVI阳性时,其诊断淋巴结转移的AUC为0.854,敏感性为79.7%,特异性为78.1%,表明ctEMVI在胃癌淋巴结转移方面诊断价值较高,其诊断胃癌淋巴结转移的敏感性和准确性均优于淋巴结短径。因此我们认为ctEMVI可作为一个重要的影像评价指标用于淋巴结转移的诊断,以弥补淋巴结短径在诊断淋巴结转移方面敏感性低的缺陷。
有研究[15]表明,N0期患者5年总生存率为86.1%,N1、N2和N3期患者的5年总生存率分别急剧下降至58.1%、23.3% 和5.9%。因而术前明确淋巴结是否转移对患者治疗方式的选择具有重要意义。对于淋巴结转移患者可行围手术期化疗和放疗以提高患者临床预后[2]。所以期待ctEMVI在胃癌患者的术前影像评估中得到广泛应用,从而对临床选择合适治疗方案及改善患者预后提供重要帮助。
本研究存在的局限性:①本研究入选患者包括早期和进展期胃癌患者,这可能会导致潜在的混杂因素;②本研究需进一步探讨 ctEMVI与其他影像评价方法在判断淋巴结转移方面联合应用的价值;③本研究 ctEMVI尚无相对应的病理学证据支持,今后仍需深入研究。
综上所述,ctEMVI是胃癌淋巴结转移的独立影响因素,在诊断淋巴结转移方面具有重要价值,可作为重要的影像学评价指标而广泛应用于临床,为临床指导治疗及判断预后提供重要帮助。
-
表 1 淋巴结转移组与非淋巴结转移组临床病理特征比较
Table 1 Clinicopathological features of lymph node versus non-lymph node metastasis groups
指标 组别 统计检验 淋巴结转移组(n=64)(%) 非淋巴结转移组(n=41)(%) $t/\chi^2 $ P 年龄/岁 63.3±10.40 62.1±10.65 0.605 0.546 性别 男 44(68.7) 28(68.3) 0.002 0.961 女 20(31.3) 13(31.7) 肿瘤位置 胃底 10(15.6) 2(4.8) 4.786 0.091 胃体 21(32.8) 13(31.7) 胃窦 33(51.6) 26(63.5) 分化程度 低分化 34(53.1) 14(34.2) 3.695 0.158 中分化 26(40.6) 24(58.5) 高分化 4(6.3) 3(7.3) 脉管侵犯 39(60.9) 9(21.9) 15.306 <0.001 肿瘤大小/cm <5 23(35.9) 31(75.6) 15.746 <0.001 >5 41(64.1) 10(24.4) ctEMVI 阴性 13(20.3) 32(78.1) 34.016 <0.001 阳性 51(79.7) 9(21.9) CT转移性淋巴结 阴性 28(43.8) 33(80.5) 13.855 <0.001 阳性 36(56.2) 8(19.5) 表 2 logistic回归分析胃癌淋巴结转移的影响因素
Table 2 Logistic regression analysis of factors affecting lymph node metastasis in gastric cancer
指标 B WaldX2 OR 95%CI P 脉管侵犯 0.817 2.135 2.26 (0.75,6.76) 0.144 肿瘤大小 0.912 2.713 2.49 (0.84,7.36) 0.100 ctEMVI 1.916 12.207 6.79 (2.31,19.89) <0.001 CT转移性淋巴结 1.087 3.684 2.97 (0.97,8.99) 0.055 表 3 ctEMVI与淋巴结短径对胃癌淋巴结转移的诊断价值比较
Table 3 Diagnostic value of ctEMVI and lymph node short diameter on lymph node metastasis of gastric cancer
指标 敏感性/% 特异性/% 阳性预测值/% 阴性预测值/% 准确性/% ctEMVI 79.7(51/64) 78.1(32/41) 85.0(51/60) 71.1(32/45) 79.1(83/105) 淋巴结短径 56.2(36/64) 80.5(33/41) 81.8(36/44) 54.1(33/61) 65.7(69/105) P 0.004 0.785 0.665 0.785 0.031 -
[1] 王凌云, 张阳, 陈勇, 等. 双能CT影像组学模型评估进展期胃癌新辅助化疗后浆膜侵犯的临床价值研究[J]. CT理论与应用研究, 2021, 30(5): 591−602. DOI: 10.15953/j.1004-4140.2021.30.05.07. WANG L Y, ZHANG Y, CHEN Y, et al. Clinical value of applying dual-energy CT radio-mics Model to evaluate serosal invasion of advanced gastric cancer after neoadjuvant chemotherapy treatment[J]. CT Theory and Applications, 2021, 30(5): 591−602. DOI: 10.15953/j.1004-4140.2021.30.05.07. (in Chinese).
[2] LI H L, LIN D D, YU Z, et al. A nomogram model based on the number of examined lymph nodes-related signature to predict prognosis and guide clinical therapy in gastric cancer[J]. Frontiers in Immunology, 2022, 13: 947802. DOI: 10.3389/fimmu.2022.947802.
[3] ZHU Y J, ZHOU Y T, ZHANG W, et al. Value of quantitative dynamic contrast-enhanced and diffusion-weighted magnetic resonance imaging in predicting extramural venous invasion in locally advanced gastric cancer and prognostic significance[J]. Quantitative Imaging in Medicine and Surgery, 2021, 11(1): 328−340. DOI: 10.21037/qims-20-246.
[4] SONZ P, SUPREETA A, SMRUTI M, et al. Extramural vascular invasion as an independent prognostic marker in locally advanced rectal cancer: Propensity score match pair analysis[J]. Abdominal Radiology, 2022, 47(11): 3671−3678. DOI: 10.1007/s00261-022-03608-z.
[5] 李修奎, 孟德杰, 等. 术前ceMDCT用于原发性胃癌壁外静脉血管侵犯诊断与术后无病生存的相关性分析[J]. 现代消化及介入诊疗, 2020, 25(10): 1367−1371. [6] CHEN Z, HU D, YE G N, et al. Quantitative evaluation of extramural vascular invasion of rectal cancer by dynamic contrast-enhanced magnetic resonance imaging[J]. Contrast Media Molecular Imaging, 2022, 56: 6.
[7] YOU J M, KIM T U, KIM S, et al. Preoperative N stage evaluation in advanced gastric cancer patients using multidetector CT: Can the sum of the diameters of metastatic LNs be used for Nstage evaluation[J]. Clinical Radiology, 2019, 74(10): 782−789. DOI: 10.1016/j.crad.2019.06.030.
[8] 柴亚如, 高剑波, 岳松伟, 等. 能谱CT多参数成像预测胃癌淋巴结转移的应用价值[J]. 中华消化外科杂志, 2021, 20(2): 240−245. CHAI Y R, GAO J B, YUE S W, et al. Application value of spectral CT multi-parameter imaging in predicting gastric cancer lymph node metastasis[J]. Chinese Journal of Digestive Surgery, 2021, 20(2): 240−245. (in Chinese).
[9] 胡顺航, 周英发. 早期胃癌淋巴结转移的相关危险因素研究[J]. 临床研究, 2022, 4(30): 21−24. HU S H, ZHOU Y F. Study on the related risk factors of lymph node metastasis in early gastricCancer[J]. Clinical Research, 2022, 4(30): 21−24. (in Chinese).
[10] FILIPPO C, RICCARDO B Q, VALENTINA M, et al. Predictors of metastatic lymph nodes at preoperative staging CT in gastric adenocarcinoma[J]. Tomography, 2022, 8(3): 1196−1207. DOI:10.3390/tomography8030 098.
[11] HASEGAWA S, YOSHIKAWA T, JUNYA S, et al. A prospective validation study to diagnose serosal invasion and nodal metastases of gastric cancer by multidetector-row CT[J]. Annals of Surgical Oncology, 2013, 20(6): 2016−22. DOI: 10.1245/s10434-012-2817-1.
[12] WEI J T, ZHANG Y N, WANG Z L, et al. Identification of lymph node metastasis by computed tomography in early gastric cancer[J]. Chinese Journal of Cancer Research, 2021, 33(6): 671−681. DOI: 10.21147/j.issn.1000-9604.2021.06.04.
[13] ABE T, YASUI M, IMAMURA H, et al. Combination of extramural venous invasion and lateral lymph node size detected with magnetic resonance imaging is a reliable biomarker for lateral lymph node metastasis in patients with rectal cancer[J]. World Journal of Surgical Oncology, 2022, 20(1): 5. DOI: 10.1186/s12957-021-02464-3.
[14] TAN C H, VIKRAM R, BOONSIRIKAMCHAI P, et al. Extramural venous invasion by gastrointestinal malignancies: CT appearances[J]. Abdominal Radiology, 2011, 36(5): 491−502.
[15] ZHANG L Y, ZANG L, SUN J, et al. Long-term outcomes of laparoscopy-assisted gastrectomy for T4a advanced gastric cancer: A single-center retrospective study[J]. Surgical laparoscopy Endoscopy Percutaneous Techniques, 2019, 29(6): 476−482. DOI: 10.1097/SLE.0000000000000684.
-
期刊类型引用(1)
1. 朱明古,刘春燕,刘素娟,戈琦,罗肇文. 醋酸染色联合蓝激光成像技术对早期胃癌的诊断价值. 中国医药指南. 2024(14): 1-4 .  百度学术
百度学术
其他类型引用(0)



 下载:
下载: